- Received July 31, 2024
- Accepted September 26, 2024
- Publication February 15, 2025
- Visibility 5 Views
- Downloads 0 Downloads
- DOI 10.18231/j.ijogr.2025.028
-
CrossMark
- Citation
A case series on navigating ovarian cysts during pregnancy assess the outcomes
Introduction
Ovarian cysts in pregnancy are not uncommon. According to a recent study, adnexal masses are discovered in 1 per 76–1 per 2328 deliveries.[1] Most ovarian cysts encountered are functional cysts of the ovary. Other cysts commonly seen are benign cystic teratomas, serous cystadenomas, para-ovarian cysts, mucinous cystadenomas, and Endometrioma. Most of these will resolve after the first 14-16 weeks of gestation but about 65-80% are asymptomatic and persist until after delivery.[1] Cysts present after 16 weeks are non-functional and will require further management. Complications of ovarian cysts in pregnancy include torsion, rupture, infection, malpresentation of fetus at term, and rarely obstructed labor. Early diagnosis, proper follow-up, and timely decision on management can aid in carrying the pregnancy on until term, for good maternal and fetal outcomes.
Case Series
Case 1
26-yr-old Primigravida presented at 27 weeks of gestational age with abdominal pain since 15 days. The patient was apparently normal 15 days Back and then developed lower abdominal pain, not radiating, No aggravating or relieving factors. Not associated with vomiting or loose stools. No history of fever or UTI symptoms. Ultrasound showed a 5.5 x 4.8 cm simple right adnexal cyst, with no signs of torsion. Investigations showed CA125 was 34.5, CEA was <0.31 and Sr. LDH was 142. The patient was managed conservatively with analgesics and antenatal steroid coverage was given and discharged. She was then admitted at 38 weeks 1 day and she underwent elective LSCS with cystectomy under spinal anesthesia. Histopathology showed a hemorrhagic cyst with decidual tissues with areas of hemorrhage. The postnatal period was uneventful.
Case 2
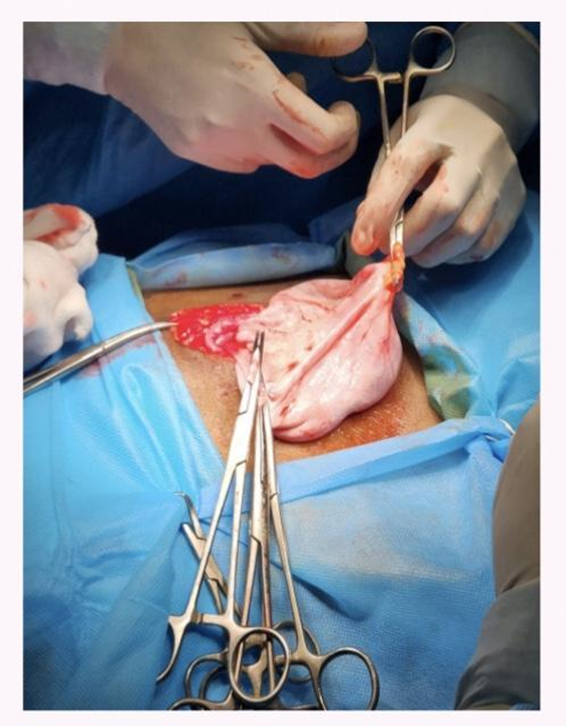
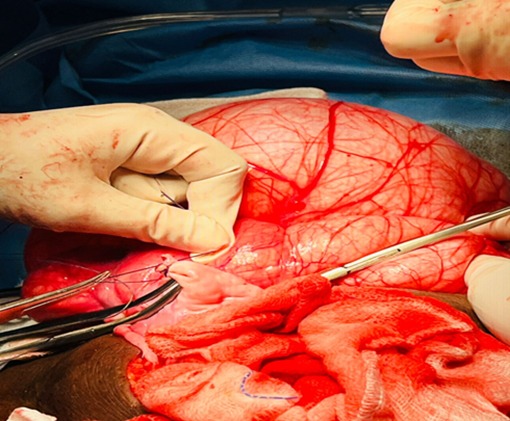
24-year-old Primigravida at 14 weeks gestational age presented with complaints of abdominal pain. No aggravating or relieving factors. Not associated with vomiting or loose stools. No history of fever or UTI symptoms. The patient had a history of old pulmonary tuberculosis and anti-tuberculosis treatment was completed. On abdominal examination, a cystic mass was palpable in the right iliac fossa of size 10x8cm, non-tender. NT scan was normal with NT 1.2 mm, however a right ovarian cyst of 15.2x 11x 6.5cm with no signs of torsion was seen in the right adnexa. Investigations revealed CA125 - 7.7, CEA – 0.96, Sr. LDH – 116. As cited in the [Figure 1] patient was taken up for Laparotomy and Right salpingo-oophorectomy was done under general anaesthesia. Histopathology showed benign mucinous cystadenoma. The remainder of the pregnancy period was uneventful and the patient had a normal vaginal delivery at term (39 weeks).
Case 3
23-year-old primigravida at 14 weeks 5 days gestational age presented with a chief complaint of abdominal pain associated with vomiting, no history of fever or UTI symptoms. A dating scan showed a large simple cystic pelvic abdominal mass of size 9.2 x 12 cm. Follow-up ultrasound at 14 weeks showed an increase in the size of the cyst to 12x 18 cm. The patient gave a history of use of letrozole for ovulation induction. She had no significant medical, surgical, or family history. On abdominal examination, the uterus was just palpable, and a cystic mass of 28 weeks in size was palpable, occupying all quadrants. Investigations showed CA 125 – 11.3, CEA – 0.32, LDH 224, s. AFP<0.495. The patient was taken up for Laparotomy and para ovarian cystectomy was done under. Histopathology showed a simple serous cyst. The postoperative period was uneventful. The patient came at 28 weeks with preterm prelabour rupture of membranes, labor progressed spontaneously and she had assisted breech delivery of an 800gm fetus. The baby died on day 15 of life.
Case 4
A 19-year-old Primi at 6 weeks 3 days gestational age presented with a complaint of lower abdominal pain sharp in nature, not radiating, and not associated with any other factors. No other aggravating or relieving factors. She had no significant medical, surgical, or family history. On examination soft diffuse tenderness is present. On pervaginal examination cervix and vagina healthy, os closed. Ultrasound showed an approximately 9x7cm right-sided cyst with evidence of torsion. The patient underwent emergency laparotomy— right oophorectomy for right ovarian torsion under spinal anesthesia. Histopathological examination showed a simple serous cyst. She had a spontaneous miscarriage at 9 weeks.
Case 5
A 31-year-old G4P2L1A1 / prev 2 LSCS presented at 20 weeks with a complaint of pain abdomen, not radiating not associated with any other factors. No other aggravating or relieving factors. She had no significant medical, surgical, or family history. On examination, uterus corresponds to 20 weeks with a good fetal heart rate. Ultrasound showed an ovarian cyst of size 6x7cm along with cholelithiasis, patient underwent laparoscopic cholecystectomy with ovarian cystectomy. Histopathological examination showed a simple serous cyst.
Discussion
Adnexal masses may be detected in 1-2% of pregnant women during routine ultrasound and they may or may not persist.[2] The most common ovarian masses encountered during pregnancy are functional cysts of the ovary. The other ovarian masses are hemorrhagic cysts, leiomyomas, and hyperstimulated ovaries. Other uncommon adnexal lesions specific to pregnancy are hyperreactio luteinalis, theca lutein cysts with moles, luteomas, teratomas, endometriomas, hydrosalpinx, cystadenomas and cystadenocarcinomas.[2]
The corpus luteum of pregnancy usually persists for 8–9 weeks. It produces progesterone and maintains the pregnancy until the placenta takes over. When the corpus lute up fails to resort, functional cysts may occur.[3], [4] Hormonal changes in pregnancy can cause follicular cysts. Bleeding into simple cysts may be seen as hemorrhagic cysts.[4]
In patients with a history of ovulation induction, hyperstimulated ovaries can also be seen in pregnancy, though this usually resolves spontaneously.[4], [5] In pregnancies with high hCG levels like multiple pregnancies, gestational trophoblastic disease, hyperthyroidism, and hyperreactio luteinalis may occur.[3]
Other common adnexal lesions in pregnancy include para-ovarian cysts, hydrosalpinx, and leiomyomas.[3], [6] In the case of leiomyomas, symptoms may mimic those of acute torsion of ovarian cysts, as there may be an increase in the size of the fibroid under the influence of pregnancy-related hormones which can lead to red degeneration.[3], [4]
As in non-pregnant women, the most common benign ovarian tumors are cystadenomas.[3] Benign to malignant transformation is extremely rare, but it has been reported.[4] Malignant ovarian cysts occur in about one per 12,000–47,000 pregnancies.[7] Adnexal masses first diagnosed in pregnancy have a 1% risk of malignancy.[2] In pregnancy, dysgerminoma is more common than epithelial ovarian tumors.[3]
In 2008, Glanc et al found that a simple cyst of 3 cm or more usually starts to regress after 10 weeks, such that only 1.5% of the cyst may remain by 14 weeks.[5] Zanetta et al found that in the case of pregnant women with ovarian cysts of at least 3cm, by the end of the pregnancy, there was either complete resolution or at least 50% regression of cyst size in 54.5% of patients, irrespective of cyst type.[8]
Complications that may be encountered in the case of large ovarian cysts include the risk of torsion, labor obstruction, and even rupture.[3], [4], [9] There is a 1% higher chance of torsion in pregnant patients compared to nonpregnant patients, the highest being in the first trimester and with the risk-reducing as the gestational age increases.[3], [4] Other complications include infection of the cyst, malignancy, impaction of the cyst in the pelvis, and malpresentation of the fetus.
The management of ovarian cysts in pregnancy mainly depends on the type of cyst, the size of the cyst, the period of gestation, and whether the patient is symptomatic or asymptomatic. Investigations play a major role in management. The advances in ultrasound have vastly improved diagnostic ability and almost all adnexal lesions can be identified. Features of malignancy like thick-walled cysts, solid or mixed cystic and solid mass, internal papillary excrescences, and free fluid in the abdomen may raise concern, wherein an MRI can be done for further evaluation.[10]
Tumor markers like CA-125, AFP, beta hCG, Inhibin B, and AMH, which are commonly used in case of non-pregnant patients for differentiating benign and malignant lesions, have a limited role in pregnancy as they increase in normal pregnancy as well, especially in the first trimester due to trophoblast invasion and in the third trimester due to detachment of the placenta.[11] Therefore, CA125, a higher cut-off value for CA-125 can be used to diagnose malignancy in pregnant patients. Markers like CEA, CA 19-9, and CA 15-9 are not influenced by pregnancy and are useful and reliable tumor markers.[12]
Once diagnosed, management of ovarian cysts in pregnancy should be individualized. There are no clear-cut guidelines on the treatment of ovarian cysts in pregnancy and it is still a topic of hot debate. It is usually seen that asymptomatic simple cysts smaller than 6 cm, are usually benign, and thus can be managed conservatively with close US follow‐ups.[6] As found by Zanetta et al, only 3 of 79 patients with adnexal cysts in pregnancy required surgical management in view of torsion, while all other patients were followed up with serial ultrasound and there was either complete resolution or at least 50% regression of cyst size in 54.5% of patients, irrespective of cyst type.[8]
Surgical intervention, either by laparotomy or laparoscopy, is usually indicated in cases where the patient is symptomatic, in case of large size of cyst (8-10cm), enlargement or persistence of cyst, rupture of cyst, torsion, hemorrhage, or increased suspicion of malignancy.[1], [13], [11] The best time for surgery is usually during the second trimester.[6] By the second trimester, most functional cysts would have regressed or disappeared and surgery may not be needed. However, in the case of persistent cysts, surgery in the second trimester has a lower chance of spontaneous abortions (a chance of about 15% in the first trimester).[2] However, surgery in the third trimester is avoided as the large uterus makes such surgery difficult and there is an increased risk of preterm delivery and placental abruption. Therefore, it might be better to proceed with expectant management till the postpartum period or to plan for a cesarean delivery with cystectomy. However, in case of acute symptoms, surgery can be performed at any gestational age after proper preoperative counselling.[2]
The mode of surgery, by Laparoscopy or Laparotomy, depends on patient criteria and surgeon experience. Usually, second-trimester pregnancy with a cyst having a low risk of malignancy can be taken up for laparoscopy.[13] Laparoscopy warrants shorter hospital stay, rapid post-operative recovery, and subsequent successful pregnancies.[14] In a study by Carter et al, post-operative stay for patients undergoing laparoscopy was 1 day compared with 4.4 ± 1.1 days in the laparotomy group, with good pregnancy outcomes in both groups.[14] Though laparoscopy allows for early ambulation, reduced pain-reliant requirements and shorter hospital stays, the effect of CO2 in the etiology of fetal acidosis is still unknown and requires further study.[11], [15]
In the case of malignant ovarian cysts, the extent of surgery was determined by intraoperative findings. Most patients were detected at an early stage which may be attributed to routine screening antenatal ultrasounds.[1] Chemotherapy can also be given safely when indicated without any fetal or maternal adverse effects.[1] Malignant ovarian cysts in pregnancy are rare and the mother should be counseled regarding the risk of thromboembolic events, cesarean section, hysterectomy, and preterm birth.[16]
In the case of pregnancy and fetal outcomes, it is difficult to establish any effect of the adnexal lesion itself on pregnancy or whether the effects were due to the treatment of the mass. However, it is proved that surgical intervention for benign adnexal masses in pregnancy has a higher risk of preterm deliveries and low neonatal birth weights.[13] As evidenced by Case 3 in this series, preterm birth may be attributed to increased stress exacted on the pregnancy by the surgery.
Conclusion
Ovarian cysts or masses during pregnancy should be accurately evaluated to decide the most appropriate treatment option. Ultrasound and MRI are safe and they help to distinguish between benign and malignant lesions. A wait-and-watch strategy can be advised for an ovarian cyst with benign features. However, cysts with septations, solid components, papillae, or nodules, or when persisting after 16 weeks of pregnancy or with enlargement should be further investigated and managed. Treatment options should be discussed for each patient individually, depending on cyst features and the duration of the pregnancy. Both laparotomy and laparoscopy can be performed considering the tumor diameter, gestational age, and surgical expertise.
Source of Funding
None.
Conflicts of Interest
None.
Acknowledgements
None.
References
- P Aggarwal, S Kehoe. Ovarian tumours in pregnancy: A literature review. Eur J Obstet Gynecol Reprod Biol 2011. [Google Scholar]
- G Chiang, D Levine. Imaging of adnexal masses in pregnancy. J Ultrasound Med 2004. [Google Scholar]
- M Yacobozzi, D Nguyen, D Rakita. Adnexal masses in pregnancy. Semin Ultrasound CT MR 2012. [Google Scholar]
- N Schwartz, I E Timor-Tritsch, Wang E. Adnexal masses in pregnancy. Clin Obstet Gynecol 2009. [Google Scholar]
- P Glanc, S Salem, D Farine. Adnexal masses in the pregnant patient: A diagnostic and management challenge. Ultrasound Q 2008. [Google Scholar]
- AM Hakoun, I Aboual-Shaar, KJ Zaza, H Abou-Al-Shaar, MNA Salloum. Adnexal masses in pregnancy: An updated review. Avicenna J Med 2017. [Google Scholar]
- WJ Garrett, M Coppleson, RJF Mclnerney. Ultrasound and ovarian cysts. Med J Aust 1990. [Google Scholar]
- G Zanetta, E Mariani, A Lissoni, P Ceruti, D Trio, N Strobelt. A prospective study of the role of ultrasound in the management of adnexal masses in pregnancy. BJOG 2003. [Google Scholar]
- CL Patton. Adnexal tumors in pregnancy. Surg Gynecol Obstet 1906. [Google Scholar]
- K Togashi. Ovarian cancer: the clinical role of US, CT, and MRI. Eur Radiol 2003. [Google Scholar]
- K Hoover, TR Jenkins. Evaluation and management of adnexal mass in pregnancy. Am J Obstet Gynecol 2011. [Google Scholar]
- A Sarandakou, E Protonotariou, D Rizos. Tumor markers in biological fluids associated with pregnancy. Crit Rev Clin Lab Sci 2007. [Google Scholar]
- GS Leiserowitz, G Xing, R Cress, B Brahmbhatt, JL Dalrymple, H Smith. Adnexal masses in pregnancy: how often are they malignant?. Gynecol Oncol 2006. [Google Scholar]
- JF Carter, DE Soper. Operative laparoscopy in pregnancy. JSLS 2004. [Google Scholar]
- JL Whiteside, HL Keup. Laparoscopic management of the ovarian mass: A practical approach. Clin Obstet Gynecol 2009. [Google Scholar]
- A Nazer, N Czuzoj-Shulman, L Oddy, HA Abenhaim. Incidence of maternal and neonatal outcomes in pregnancies complicated by ovarian masses. Arch Gynecol Obstet 2015. [Google Scholar]
