- Visibility 141 Views
- Downloads 20 Downloads
- DOI 10.18231/j.ijogr.2025.008
-
CrossMark
- Citation
Evaluation of blood and blood product utilisation practice in obstetrics and gynaecology: A prospective study in a tertiary care hospital
Introduction
The leading cause of maternal death globally is major obstetric haemorrhage (MOH).[1] The cornerstone of obstetric management is blood transfusion therapy. It saves bleeding patients as a failsafe component. One of the eight components of comprehensive emergency obstetric care (EmOC) that the World Health Organization (WHO) has identified as vital to lowering the maternal mortality rate (MMR) is blood transfusion.[2]
Blood is a valuable human resource that is both limited and, given the immunological and nonimmune side effects of blood transfusion, potentially harmful. Without properly analysing the true needs, many blood requests are made as a "cushion" for patients who are in labour or who are having Caesarean sections in case of unforeseen bleeding. The guidelines for using blood for surgical purposes have not been altered in many hospitals for a very long time. Instead of using evidence-based predictions, the typical requirement for a given surgery is typically based on the subjective expectation of blood loss. Additionally, it develops as a misperception problem among operating room staff that the emergency cannot be handled by a blood bank.[3]
Increased patient morbidity and mortality, expiration of blood components, decreased blood bank inventory, blood inaccessibility during times of need, technical time wastage, increased workload, and increased transfusion costs are just a few of the severe effects of over ordering of blood and its components.[4]
The optimization of blood product utilization has emerged as a critical component of national hemovigilance programs in countries such as Belgium, Ireland, and the Netherlands. By reducing unnecessary transfusions, safeguarding blood components, and minimizing medical expenses, these nations are prioritizing efficient resource allocation and healthcare sustainability.[5]
Audits of clinical transfusion procedures have frequently emphasised the need for better knowledge regarding the prescription, identification, or administration of transfusion recipients.[6] A system for recording transfusion processes should be in place, according to the Association for the Advancement of Blood & Biotherapies (AABB). Examination of blood request forms and blood component consumption is one aspect of the system that verifies the appropriateness of blood usage in modern healthcare services.[7]
Given this background, the study's objectives are to gain knowledge of the current transfusion practises in the field of obstetrics and gynaecology at the MGM Medical College and Hospital, Navi Mumbai, and to promote the development of ethical clinical transfusion practise.
Materials and Methods
A prospective, observational study was conducted in collaboration between the Department of Transfusion Medicine and the Department of Obstetrics and Gynaecology at MGM Medical College and Hospital, Navi Mumbai over a period of 1.5 years and included all obstetrics and gynaecology patients requiring blood or blood products during this period. Data collection relied exclusively on request forms and blood bank records without direct patient interaction, emphasizing the observational nature of the study. Data were collated using Excel and analyzed with IBM SPSS version 26.
Three key indices were employed to evaluate blood utilization practices namely; Crossmatch to Transfusion Ratio (C/T ratio), Transfusion Probability (%T) and Transfusion Index (TI).
Results
During our research period, there were a total of 330 in-patients from department of obstetric and gynaecology for whom a request for blood transfusion was made. Out of the 330, 200 patients (60.6%) received transfusions. The total number of units that were requested for these 330 patients were 745 units, out of which 549 units (73.6%) were transfused.
The most transfused blood component was red blood cells, with 268 units accounting for 48.8% of the total, followed by fresh frozen plasma with 222 units or 40.4%, and random donor platelets with 56 units, making up 10.2%.
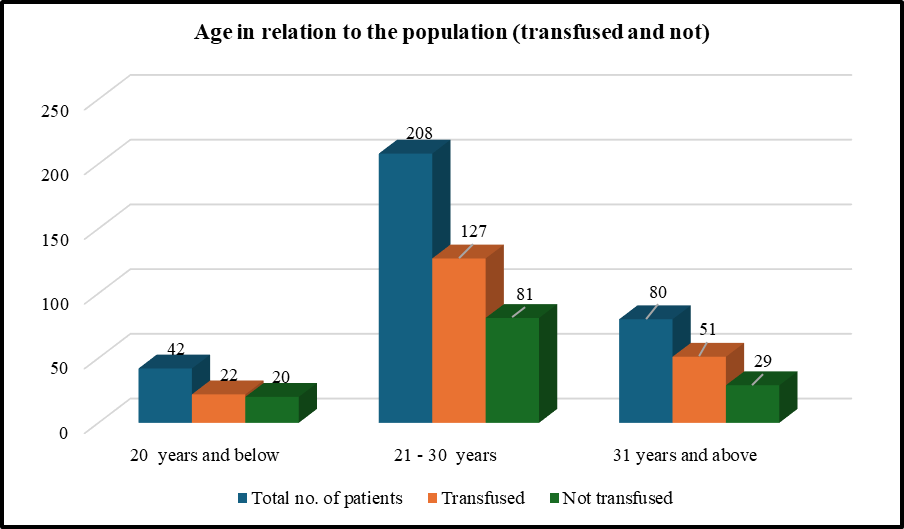
In the study, age of patients ranged from 17 years to 74 years. The majority of the study population was between the ages of 21 and 30 years of age. As shown in [Figure 1], the majority of individuals who received transfusions, accounting for 74.5% (127 patients out of 208), were in the age group of 21 to 30 years. The age group of 20 years and younger had the highest percentage of individuals who did not receive transfusions at 47.6% (20 patients out of 42).
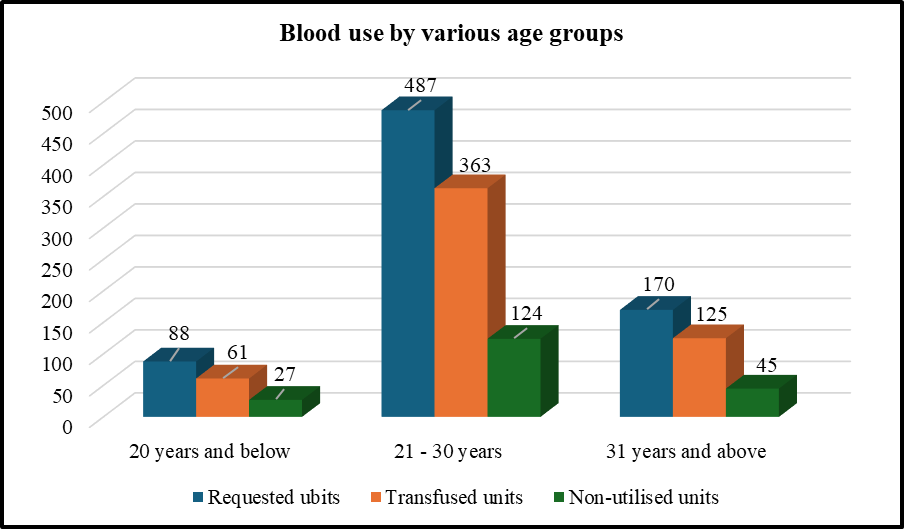
[Figure 2] shows the age based distribution of number of units requested and their utilisation. The age group from 21 to 30 years old saw the highest utilization of blood components and transfusions with 363 transfused units out of 487 requested units.
Out of 330 patients, 215 instances (65.2%) involved multiparous women, which were transfused 176 units of red blood cells (RBC), 44 units of random donor platelets (RDP), 144 units of fresh frozen plasma (FFP), and 1 unit of cryoprecipitate. Primiparous women accounted for 115 cases (34.8%) and received 92 units of RBC, 12 units of RDP, 78 units of FFP, and 2 units of cryoprecipitate as shown in [Table 1].
|
Parity |
No. of patients |
Requested units |
Transfused units |
||||||
|
PRC |
RDP |
FFP |
CRYO |
PRC |
RDP |
FFP |
CRYO |
||
|
Primipara |
115 |
153 |
14 |
80 |
2 |
92 |
12 |
78 |
2 |
|
Multipara |
215 |
289 |
50 |
156 |
1 |
176 |
44 |
144 |
1 |
The most frequent diagnosis in the study population was anemia complicating pregnancy (170 cases, 51.5%), which had used 131 units of red blood cells with a maximum utilization rate of 58.2%. The next most common diagnosis was Caesarean section (86 cases, 26.1%), which used 39 units of red blood cells with a utilization rate of 41.1%. Ectopic pregnancy cases made up 4.5% (15 cases) of the study's participants and consumed 7.8% of all the red blood cells that were transfused.
To evaluate the appropriateness of red blood cell transfusions, number of units requested as well as transfused for different haemoglobin ranges of the study population were studied as shown in [Table 2].
|
Haemoglobin range (in gm/dL) |
No. of patients |
Units Requested |
Units Transfused |
|
< 6 |
30 |
60 |
52 |
|
6 – 7 |
42 |
66 |
53 |
|
7 – 8 |
44 |
67 |
59 |
|
8 – 10 |
71 |
89 |
54 |
|
> 10 |
143 |
160 |
50 |
[Table 3] shows the maximum blood order schedule (MBOS) along with cross match to transfusion ratio (C/T ratio) for different indications and diagnosis observed in our present study.
|
Diagnosis |
C/T ratio |
TI |
Maximum blood order (TI x 1.5) |
|
Abortion |
1.06 |
2.3 |
3.4 |
|
Abruptio Placenta |
1 |
4 |
6.0 |
|
Anaemia |
1.72 |
0.8 |
1.2 |
|
Cervical carcinoma |
1 |
1 |
1.5 |
|
Eclampsia |
1.16 |
1.7 |
2.5 |
|
Ectopic Pregnancy |
1.14 |
1.6 |
2.4 |
|
Fibroid |
2 |
0.7 |
1.1 |
|
Hysterectomy |
2 |
0.8 |
1.2 |
|
IUFD |
1 |
1 |
1.5 |
|
LSCS |
2.44 |
0.5 |
0.7 |
|
Ovarian cyst |
1.33 |
1 |
1.5 |
|
Placenta previa |
1 |
2.5 |
3.8 |
|
PPH |
1.5 |
0.8 |
1.2 |
|
RPOC |
1 |
1.5 |
2.3 |
|
Trophoblastic disease |
1 |
1 |
1.5 |
|
Uterine malignancy |
1 |
1 |
1.5 |
[Table 4] provides the incidence for single unit transfusions observed in our study along with the haemoglobin range of patients receiving them.
|
Single units |
Hemoglobin range (mg/dL) |
||||||
|
No. of cases transfused |
No. of units transfused |
No. of cancelled units |
<6 |
6-7 |
7-8 |
8-10 |
>10 |
|
101 |
101 |
125 |
11 |
19 |
26 |
27 |
18 |
Discussion
The critical evaluation of blood transfusion practices within obstetrics and gynaecology at MGM Medical College and Hospital, Navi Mumbai, reveals a complex interplay of clinical need, demographic factors, and transfusion outcomes. This study, through a prospective, observational lens, has dissected the utilization patterns, efficiency of blood ordering, and the appropriateness of transfusions against established guidelines, providing a nuanced understanding of transfusion medicine in this specialized setting.
The present study's findings highlight a significant transfusion rate of 60.6% among obstetrics and gynaecology in-patients, reflecting the critical need for transfusion services in managing complex obstetric cases, which often present at tertiary centers like ours. This rate is notably higher than some previous studies, indicating a possible reflection of our hospital's status as a referral centre for high-risk pregnancies.
The demographic distribution, particularly the concentration of transfusion needs within the 21-30 age group, aligns with the global understanding that reproductive age women are a critical demographic in obstetric care. This group accounted for the highest blood component consumption, emphasizing the importance of focused transfusion support and management strategies for this demographic. For the primipara and multipara, the red cell component utilisation was 92 RBC units (34.3%) and 176 units (65.7%), respectively. A research by Osaheni et al[8] revealed that 44.4% of primipara were at risk for transfusion.
The study's exploration of blood utilization indicators, such as the Crossmatch to Transfusion Ratio (C/T Ratio) of 1.65, provides evidence of a relatively efficient blood ordering practice within the context of emergency obstetric care, although there is room for improvement when compared to other settings or international benchmarks. [Table 5] shows a comparative analysis of C/T ratio across different regions and time periods.
|
Author |
Year of study |
Study population |
C/T ratio |
|
Present study |
2021 |
330 |
1.65 |
|
Goundan et al[9] |
2011 |
1769 |
5.46 |
|
Oluwarotimi et al[10] |
2010 |
1056 |
7.4 |
|
Khan et al[11] |
2002 |
126 |
9.7 |
|
Kameni et al[12] |
1988 |
6003 |
2.9 |
Our findings also shed light on the appropriateness of transfusions, revealing that a considerable proportion of transfusions may not align perfectly with recommended guidelines, such as those from the (Royal College of Obstetricians and Gynaecologists) RCOG. Approximately 29% of transfusions were deemed inappropriate, indicating a potential area for clinical improvement and education. According to a research by Osman et al[13] 46% of transfusions were unsuitable. According to Parker et al[14] inappropriate transfusions were 31% in patients with Haemoglobin of 7 gms% in the absence of ongoing bleeding in asymptomatic anaemic persons.
The practice of single-unit transfusions, observed at a rate of 44.6% in our study, suggests a shift towards more conservative transfusion strategies, which is a positive trend in reducing the risks associated with allogeneic blood transfusions (ABT). Studies by Sabeen Afzal,[15] Khan et al[11] and Ozumba et al[16] reported single unit transfusion rates of 11.1%, 66.2%, and 43.1%, respectively. The emphasis on early diagnosis and management of anaemia in pregnancy could further refine transfusion practices, reducing the need for multiple transfusions and enhancing patient outcomes.
Conclusion
By aligning more closely with established guidelines, optimizing blood utilization, and focusing on demographic-specific needs and appropriateness, we can enhance patient care, reduce risks, and manage the blood supply more effectively. Future directions should include targeted educational initiatives, the development of more nuanced transfusion protocols, and continued research into transfusion outcomes to ensure that blood, as a scarce and life-saving resource, is used to its fullest potential while minimizing risks to patients.
Source of Funding
None.
Conflict of Interest
None.
References
- D Adukauskiene, A Veikutiene, A Adukauskaite, V Veikutis, K Rimaaitis. The usage of blood components in obstetrics. Medicina (Kaunas) 2010. [Google Scholar]
- . Guidelines for Monitoring the Availability and Use of Obstetric Services. 1997. [Google Scholar]
- JD Sweeny, Y Rizk. . Clinical Transfusion Medicine 1999. [Google Scholar]
- RB Basnet, D Lamichhane, VK Sharma. A Study of lood Requisition and ransfusion Practice in Surgery at ir Hospital. Postgrad Med J NAMS 2009. [Google Scholar]
- HW Reesink, S Panzer, CA Gonzalez, N Lena, P Muntaabski, S Gimbatti. Haemovigilance for the optimal use of blood products in the hospital. Vox Sang 2010. [Google Scholar]
- P Clarke, I Rennie, S Rawlinson. Quality improvement report: Effect of a formal education programme on safety of transfusions. BMJ 2001. [Google Scholar]
- P Kaur, D Basu, D Kaur, R Kaur. An Analysis of the Pattern of Blood Requisition and Utilization in a Tertiary Care Centre: Analysis of the Pattern of Blood Requisition and Utilization. Natl J Integr Res Med 2013. [Google Scholar]
- OL Lawani, CA Iyoke, AK Onyebuchi. Blood transfusion trends in obstetrics at the Federal Teaching Hospital in Abakaliki, South-East Nigeria. Int J Womens Health 2013. [Google Scholar]
- AA Kameni, GH Mcmorland, LD Wadsworth. Utilization of red blood cell transfusion in an obstetric setting. Am J Obstet Gynecol 1988. [Google Scholar]
- OI Akinola, AO Fabamwo, AO Tayo, KA Rabiu, YA Oshodi, CA Onyekwere. Evaluation of blood reservation and use for caesarean sections in a tertiary maternity unit in south western Nigeria. BMC Pregnancy Childbirth 2010. [Google Scholar]
- FA Khan, M Khan, A Ali, U Chohan. Estimation of blood loss during Caesarean Section: an audit. J Pak Med Assoc 2006. [Google Scholar]
- A Goundan, JK Kalra, A Raveendran, R Bagga, N Aggarwal. Descriptive study of blood transfusion practices in women undergoing cesarean delivery. J Obstet Gynaecol Res 2011. [Google Scholar]
- A So-Osman, J Cicilia, A Brand, M Schipperus, B Berning, S Scherjon. Triggers and appropriateness of red blood cell transfusions in the postpartum patient--a retrospective audit. Vox Sang 2010. [Google Scholar]
- J Parker, J Thomson, S Stanworth. A retrospective one-year single-centre survey of obstetric red cell transfusions. Int J Obstet Anesth 2009. [Google Scholar]
- S Afzal. A comparison of public and private hospital on rational use of blood in Islamabad. J Pak Med Assoc 2013. [Google Scholar]
- B Ozumba, H Ezegwi. Blood Transfusion and Caesarean section in a developing country. J Obstet Gynaecol 2006. [Google Scholar]
