- Received April 01, 2024
- Accepted May 06, 2024
- Publication February 15, 2025
- Visibility 21 Views
- Downloads 0 Downloads
- DOI 10.18231/j.ijogr.2025.005
-
CrossMark
- Citation
Correlation of symptoms and its effects in pelvic organ support defects by pelvic organ prolapse - Quantification {POP-Q} in a teaching institution in North Kerala, India
Introduction
Pelvic organ prolapse (POP) is a condition in which one or more of the female pelvic organs, such as the bladder, uterus, vaginal cuff, rectum, and intestine dip into the vagina.[1], [2] The muscles and tissues surrounding the uterus weakens resulting in uterine prolapse.[3] Pelvic floor dysfunction when severe can be distressing for both the individual and the health care system as a whole as the general population ages and has a lower quality of life and lower productivity. This research was planned to look into the correlation of symptoms, risk factors and the quality of life with POP-Q in pelvic organ support defects in a tertiary care center in North Kerala.
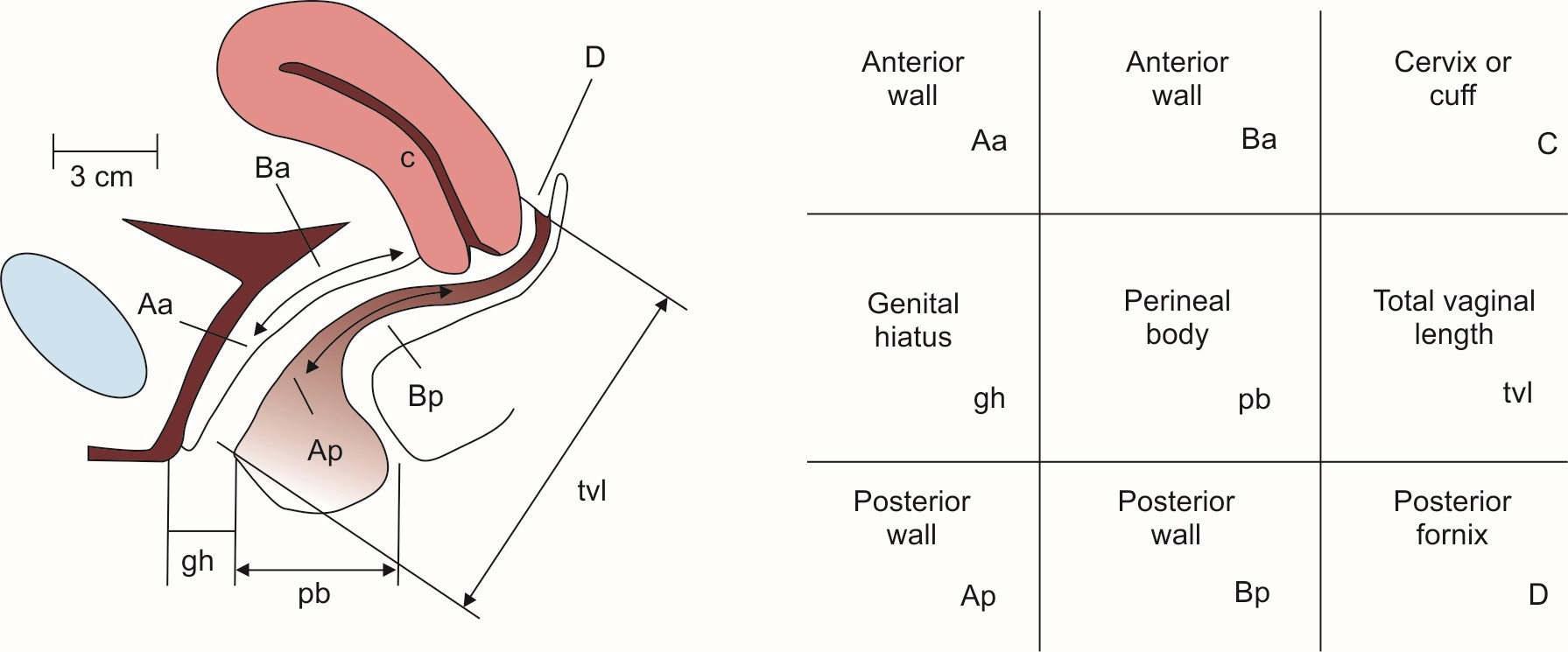
Pelvic Organ Prolapse Quantification (POP-Q System)
In 1996, the American Urogynecology Society (AUGS), the International Continence Society (ICS), and the Society of Gynecologic Surgeons reached a consensus on the need for a graded objective measure to be utilized in the evaluation of female pelvic organ prolapse. Six unique sites (Aa, Ba, C, D, Ap, and Bp) and three anatomical markers make up the measurement parameters (GH, PB, TVL).[4]
Staging of prolapse
Once all measurements have been made the stage of the prolapse can be identified in relation to hymen;
Stage 0: No prolapse is observed (points Aa, Ba, C, D, Ap and Bp are all < / = -3cm).
Stage 1: The most proximal portion of prolapse is greater than 1 cm above the level of the hymen (points Aa, Ba, C, D, Ap and Bp are all < -1cm).
Stage 2: The most proximal portion of prolapse is found between 1 cm higher than hymen and 1cm beneath hymen (points Aa, Ba, C, D, Ap, Bp can set at -1cm and +1cm).
Stage 3: The most distal part of the prolapse extends more than 1cm beneath the hymen but no further than 2 cm, resulting in no measurement larger than TVL (points Aa, Ba, C, D, Ap and Bp can be >/= +2cm and </= TVL -3cm).
Stage 4: vaginal eversion has taken place or eversion to with 2cm of TVL (points Aa, Ba, C, D, Ap and Bp can be >/= to TVL -2cm).[5]
Aims and Objectives
To know the clinical profile, risk factors and treatment modalities done for pelvic organ prolapse in women who presented with complaints of mass descending per vagina.
Materials and Methods
Ethical clearance was obtained from the institution before the start of the study.
Study design
A cross sectional observational study design done for patients presenting with complaints of pelvic organ prolapse among OP and In patients attending at KMCT Medical College, Kozhikode.
Study setting
This study was conducted in the Department of Obstetrics and Gynecology, KMCT medical college, Kozhikode.
Study duration
June 1st 2021 – May 30th 2022.
Sample size calculation
N = 4pq/d2, P = proportion or prevalence (from previous studies) = 74% Reference article[6]
d = precision = 10% q = 100-q
n = 140, a sample size of 140 was selected for this study.
Selection criteria
Newly diagnosed cases with complaints of pelvic organ prolapse with or without urinary symptoms in the recommended period, both in patients and outpatients who were willing to take part in this study and those willing for routine checkups and regular follow up were included in the study. Pregnancy, chronic illness and neurological disorders were excluded in the research.
Sampling procedure
A hospital based cross sectional study with a sample size of 140 was taken. Demographics and the history were taken a period of one year. Study population included patients attending gynecology department at the tertiary center with complaints of mass descending per vagina and related symptoms. Baseline questionnaires including age, occupation, chronic illnesses, time since menopause, hysterectomy status, constipation and occupation were enquired. Weight was measured to the nearest 0.1 kg on an electronic weighing machine with the participant dressed in indoor clothing without shoes. Height measured to the nearest 0.1 cm with a wall-mounted stadiometer. Body mass index were calculated as weight/height2.
All statistical procedures were performed using Statistical Package for Social Sciences (SPSS) 20. All quantitative variables were expressed in mean and standard Deviation. Qualitative variables expressed in percentages. Chi square test was used to test the associations. Probability value (p <0.05) was considered statistically significant.
Results
|
|
POP Q staging |
|
P value |
|||
|
Urinary symptoms |
Stage 1 |
Stage 2 |
Stage 3 |
Stage 4 |
Total |
0.935 |
|
Yes |
2(40%) |
15(39.5%) |
38(43.7%) |
5(50%) |
60(42.9%0 |
|
|
No |
3(60%) |
23(60.5%) |
49(56.3%) |
5(50%) |
80(57.1%) |
|
|
Total |
5(100%) |
38(100%) |
87(100%) |
10(100%) |
140(100%) |
The current study could not establish a relationship between the stages of prolapse with urinary symptoms of the population.([Table 1])
|
|
POP Q staging |
|
p value |
|||
|
Chronic cough or constipation |
Stage 1 |
Stage 2 |
Stage 3 |
Stage 4 |
Total |
0.253 |
|
Yes |
1(2.1%) |
12(25%) |
34(70.8%) |
1(2.1%) |
48(100%) |
|
|
No |
4(4.3%) |
26(28.3%) |
53(57.6%) |
9(9.8%) |
92(100%) |
|
|
Total |
5(3.6%) |
38(27.1%) |
87(62.1%) |
10(7.1%) |
140(100%) |
The present study had 48 persons with history of cough. 70.8% among them had stage 3 organ prolapse. But this finding did not have any significant statistical associations.([Table 2])
|
|
POP Q staging |
|
P value |
|||
|
History of heavy work load |
Stage 1 |
Stage 2 |
Stage 3 |
Stage 4 |
Total |
0.406 |
|
Yes |
1(1.4%) |
22(30.1%) |
44(60.3%) |
6(8.2%) |
73(100%) |
|
|
No |
4(6.0%) |
16(23.9%) |
43(64.2%) |
4(6%) |
67(100%) |
|
|
Total |
5(3.6%) |
38(27.1%) |
87(62.1%) |
10(7.1%) |
140(100%) |
|
|
|
POP Q staging |
|
P Value |
|||
|
Menopausal status |
Stage 1 |
Stage 2 |
Stage 3 |
Stage 4 |
Total |
0.6202 |
|
Yes |
4(80%) |
33(86.8%) |
77(88.5%) |
10(100%) |
124(88.6%) |
|
|
No |
1(20%) |
5(13.2%) |
10(11.5%) |
0(0%) |
16(11.4%) |
|
|
Total |
5(100%) |
38(100%) |
87 (100%) |
10(100%) |
140(100%) |
|
|
POP Q staging |
|
P value |
|||
|
Quality of sexual life |
Stage 1 |
Stage 2 |
Stage 3 |
Stage 4 |
Total |
<0.01 |
|
Affected |
0(0%) |
11(28.9%) |
63(72.4%) |
10(100%) |
84(60%) |
|
|
Not affected |
5(100%) |
24(63.2%) |
17(19.5%) |
0(0%) |
46(32.9%) |
|
|
Sexually not active |
0(0%) |
3(7.9%) |
7(8%) |
0(0%) |
10(7.1%) |
|
|
Total |
5(100%) |
38(100%0 |
87(100%) |
10(100%) |
140(100%) |
|
|
POP Q staging |
|
P value |
|||
|
|
Stage 1 |
Stage 2 |
Stage 3 |
Stage 4 |
Total |
0.063 |
|
Yes |
3(60%) |
26(68.4%) |
75(86.2%) |
9(90%) |
113(80.7%) |
|
|
No |
2(40%) |
12(31.6%) |
12(13.8%) |
1(10%) |
27919.3%) |
|
|
Total |
5(100%) |
38(100%) |
87(100%) |
10(100%) |
140(100%) |
|
|
POP Q staging |
|
P value |
|||
|
Presence of Rectocoele |
Stage 1 |
Stage 2 |
Stage 3 |
Stage 4 |
Total |
0.691 |
|
Yes |
3(60%) |
20(52.6%) |
44(50.6%) |
7(70%) |
74(52.9%) |
|
|
No |
2(40%) |
18(47.4%) |
43(49.4%) |
3(30%) |
66(47.1%) |
|
|
Total |
5(100%) |
38(100%) |
87(100%) |
10(100%) |
140(100%) |
|
POP Q Staging |
Conservative |
VH with PFR |
VH |
Fothergills Operation |
Total |
P value |
|
Stage 1 |
4(80%) |
0(0%) |
1(20%) |
0(0%) |
5(100%) |
<0.001 |
|
Stage 2 |
13(34.2%) |
23(60.5%) |
1(2.6%) |
1(2.6%) |
38(100%) |
|
|
Stage 3 |
7(8%) |
72(82.8%) |
4(4.6%) |
4(4.6%) |
87(100%) |
|
|
Stage 4 |
0(0%) |
10(100%) |
0(0%) |
0(0%) |
10(100%) |
|
|
Total |
17.1% |
75.0% |
4.3% |
3.6% |
100.0% |
History of heavy work load had no statistical association between POP-Q staging. (p>0.05).([Table 3])
The menopausal status of the study population did not have any significant association between POP -Q staging. 86.8% of stage 2 had attained menopause. ([Table 4])
In present study, the quality of sexual life was found to be affected in all stage 4 patients while the same was affecting comparatively lower proportion of patients in stages 2 and 3. In stage 1, the quality of sexual life was not reported to be affected by the prolapse in any of the patients.([Table 5])
In present study, the proportion of patients with cystocele was found to be gradually increasing across the stages of disease as per the POP-Q staging and the maximum proportion was seen in stage 4. ([Table 6])
It was noted that proportion of patients with rectocele was also found to be highest in stage 4, followed by stage 1. But, unlike in the case of cystocele, there was no gradual increase observed in the proportion of patients with rectocele across the stages.([Table 7])
The management of the study population had a significant statistical association with stage of the prolapse as P value < 0.05.([Table 8])
Discussion
Coming to the compartment defects, the proportion of patients with cystocele was found to be gradually increasing across all the stages of disease as per the POP-Q staging and the maximum proportion was noted in stage 4. S Kumari opined that rectocele was seen in 14.2% of cases, and cystocele in 35.7% of them. Third degree uterovaginal prolapse was the most common diagnosis among symptomatic patients.[7] Prolapse of the vault were in 11.3%. Among the cohort studied by Susan L. Hendrix et al in 2004, the proportion of cystocele was only one-third with very few in earlier stages having urinary symptoms.[8] In stage 4, half of them reported urinary symptoms. J Awwad et al, opined that POP prevalence was 20.4% for women in the 20–29 age group, 50.3% for those in the 30–39 age group, 77.2% for those in the 40–49 age group, and 74.6% for those in the 50–59 age group when stratified by life decade.[9] This suggests a plateau in prevalence in the decade following menopause. BMI: Waist circumference more than 88 cm was associated with pelvic organ prolapse according to Susan L. Hendrix et al.[8] As the waist circumference is a measure of obesity, this association is an expected one. It was observed that 52.1% were obese in present study. But, the finding from the study of DF Shalom et al was similar to that observed in present study.[10] They could not find any correlation between BMI and any POP-Q. History of comorbidities like chronic cough or mass abdomen did not turn out to be risk factors for prolapse in present study while chronic obstructive pulmonary disease and constipation were risk factors for prolapse as per Farjana Akter et al.[11] Constipation was reported to be a risk factor by Susan L. Hendrix et al also.[8] Persistent cough was a risk factor for prolapse according to Payal Rathod et al.[12] The conditions that put additional pressure on abdominal and pelvic organ for a considerable period and are established causes of pelvic organ prolapse. As per Zhiyi Li et al, pelvic organ prolapse was also linked to obesity, constipation, smoking, coughing, gynecological conditions and other physical disorders, according to multivariate logistic regression.[13] T K S Ravindran et al had reported that women who suffer from uterine prolapse had major quality of life as in stage 4 prolapse cases.[14] It had definite effects on their sexual life as well as the ability to work and support themselves, and their physical health. In present study, stage 1 in the POP- Q needed only conservative management(ring pessary application and Kegels exercise) while all other stages required vaginal hysterectomy and pelvic floor repair. This observation is similar to what was reported by Nitin Joseph et al.[6] As per them vaginal hysterectomy was the most often performed surgical treatment among their cases of pelvic organ prolapse. They could also observe that ring pessary application was the conservative management for their study participants with prolapse. Dara F. Shalom, et al noted that in the majority of cases, ring pessaries were used, and significant improvements in their health were reported following this type of management. S Kumari observed that on OPD basis, pessary application and Kegel’s were the commonest management modalities adopted.[7] J Kulkarni et al, on a “Clinical study of utero-vaginal prolapse” in Pune revealed that maximum prolapse rates -76.50% were para three and above and 85% belongs to lower socioeconomic status.[15] The chosen procedure was a vaginal hysterectomy with pelvic floor reconstruction. Fothergill's repair and Shirodkar's sling operation were next two more often done procedures. Pessary had limited role in prolapse control. But, in the study by P Rathod et al, half of the patients with pelvic organ prolapse had undergone surgical intervention.[12] This almost coincides with the finding of present study. As per Jonathan, post hysterectomy vault prolapse defects repair were 3.6 per 1000 person-years of risk. They also noted that after a hysterectomy, the cumulative risk of prolapse increases from 1% to 5% over a period of 15 years.[16]
Conclusion
Pelvic organ support defects such as cystocele and rectocele has been found to be gradually increasing across the stages of disease as per the POP-Q staging and the maximum proportion was seen in stage 4. In stage 1, the quality of sexual life was not reported to be affected by the prolapse in any of the patients (p<0.01), while stage 4 defects necessitated surgical treatment to improve the overall quality of life.
Author's Contribution
Dr Shameema Puthuprakkat has prepared the conceptual framework, designing of draft, data collection and data analysis., Dr Chellamma V K supervised and designed the study. and Dr Lisha Govind has helped in the manuscript writing and Dr Heera Shenoy T has done the final editing. Dr Naseema Beevi provided the funding.
Conflict of Interest
None declared.
Ethical Approval
The study was approved by the Institutional Ethics Committee and Institutional Research Committee of KMCT Medical College, Kozhikode.
References
- KH Choi, JY Hong. Management of pelvic organ prolapse. Korean J Urol 2014. [Google Scholar]
- MD Barber. Pelvic organ prolapse. BMJ 2016. [Google Scholar]
- VP Mazzola, NJ Mazzola, FV Mitchell, DS Fettes, HL Martone, GR D’onofrio. Uterine prolapse. Am J Surg 1953. [Google Scholar]
- . Pelvic organ prolapse quantification (POP-Q) system. 2023. [Google Scholar]
- GJA Walker, P Gunasekera. Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J 2011. [Google Scholar]
- N Joseph, C Krishnan, BA Reddy, NA Adnan, LM Han, YJ Min. Clinical Profile of Uterine Prolapse Cases in South India. J Obstet Gynaecol India 2016. [Google Scholar]
- S Kumari, I Walia, A Singh. Self-reported uterine prolapse in a resettlement colony of north India. J Midwifery Womens Health 2000. [Google Scholar]
- SL Hendrix, A Clark, I Nygaard, A Aragaki, V Barnabei, A McTiernan. Pelvic organ prolapse in the Women’s Health Initiative: gravity and gravidity. Am J Obstet Gynecol 2002. [Google Scholar]
- J Awwad, R Sayegh, J Yeretzian, ME Deeb. Prevalence, risk factors, and predictors of pelvic organ prolapse: a community-based study. Menopause 2012. [Google Scholar]
- DF Shalom, SN Lin, SS Louis, HA Winkler. Effect of age, body mass index, and parity on Pelvic Organ Prolapse Quantification system measurements in women with symptomatic pelvic organ prolapse. J Obstet Gynaecol Res 2012. [Google Scholar]
- F Akter, P Gartoulla, J Oldroyd, RM Islam. Prevalence of, and risk factors for, symptomatic pelvic organ prolapse in Rural Bangladesh: a cross-sectional survey study. Int Urogynecol J 2016. [Google Scholar]
- P Rathod, S Gaddappa, A Sonawane, R Gaikwad. Study of pelvic organ prolapse- A tertiary care experience. Eur J Mol 2022. [Google Scholar]
- Z Li, T Xu, Z Li, J Gong, Q Liu, L Zhu. An epidemiologic study of pelvic organ prolapse in rural Chinese women: a population-based sample in China. Int Urogynecol J 2019. [Google Scholar]
- TS Ravindran, R Savitri, A Bhavani. Women’s experiences of utero-vaginal prolapse: a qualitative study from Tamil Nadu, India. Safe motherhood initiatives: critical issues 1999. [Google Scholar]
- J Kulkarni, S Burute, M Maini, S Sansare. Clinical study of utero-vaginal prolapse. Int J Clin Obstet Gynaecol 2020. [Google Scholar]
- J Mant, R Painter, M Vessey. Epidemiology of genital prolapse: observations from the Oxford Family Planning Association Study. Br J Obstet Gynaecol 1997. [Google Scholar]
